WHAT IS NON-ALCOHOLIC FATTY LIVER DISEASE?
Non-alcoholic fatty liver disease (NAFLD) is a condition characterized by the accumulation of excess fat in the liver of people who drink little to no alcohol. It is becoming increasingly common in many parts of the world, especially in Western countries, and is closely associated with obesity, type 2 diabetes, and other disorders that are part of the metabolic syndrome, including hypertension and hyperlipidemia (high levels of fat in the blood). It is estimated that 20% of adults in the US have NAFLD.
NAFLD ranges in severity from simple fatty liver (steatosis), which is generally benign, to non-alcoholic steatohepatitis (NASH), a more serious form of the disease. NASH is characterized by liver inflammation and may progress to more severe liver damage, such as fibrosis (scarring of the liver), cirrhosis (advanced liver scarring that impairs liver function), and even liver cancer.
WHAT CAUSES NAFLD?
The exact cause of NAFLD is not fully understood, but it is believed to result from a combination of genetic, environmental, and lifestyle factors. Some of the key lifestyle risk factors include:
Obesity: Excess body fat, especially around the abdomen, is strongly associated with NAFLD. Obesity can increase the accumulation of fat in the liver, contributing to inflammation and liver damage.
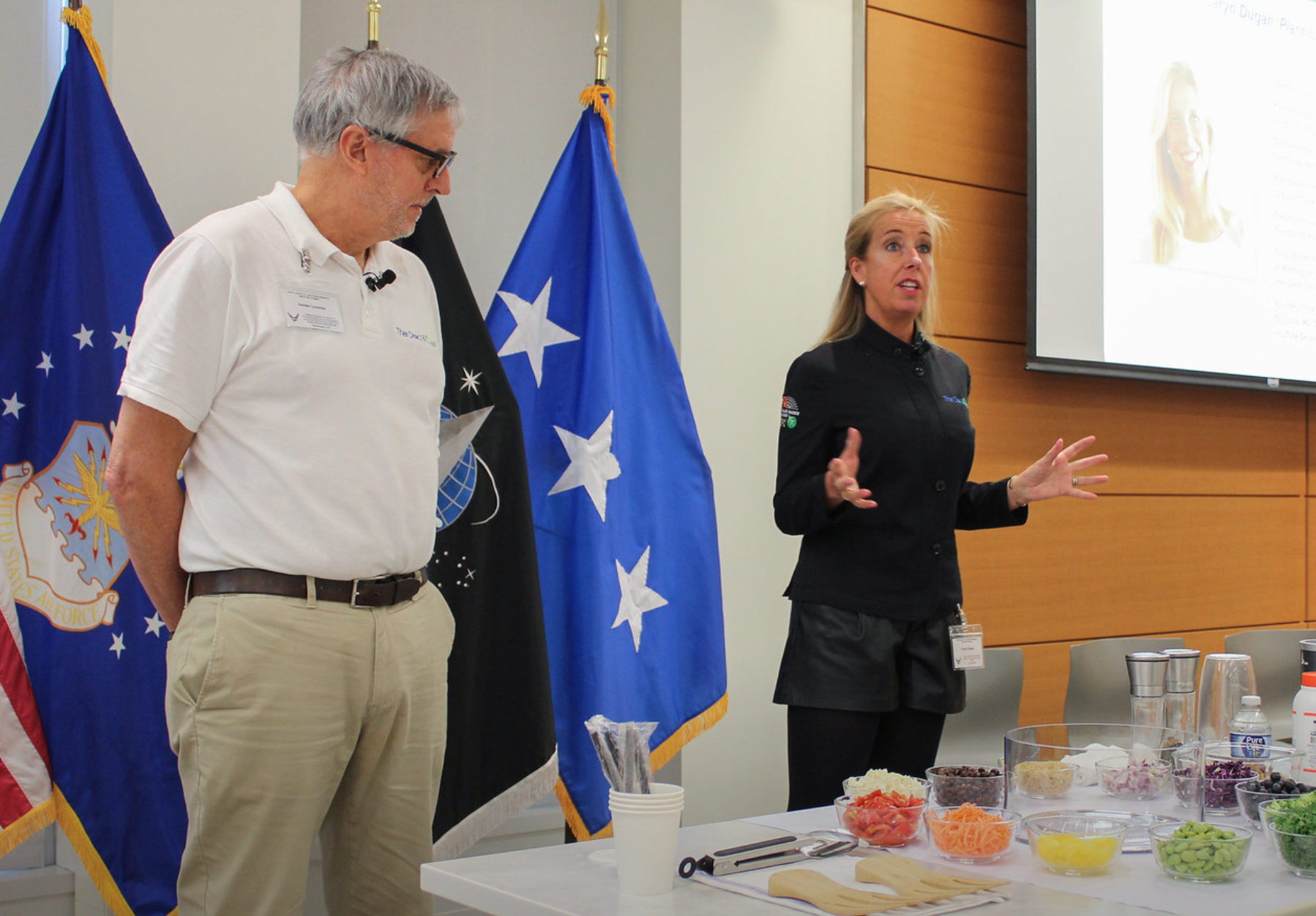
Poor Diet: A diet high in saturated fats, trans fats, refined carbohydrates, and sugars can contribute to the development of NAFLD. Such diets can promote liver fat storage and worsen insulin resistance.
Physical Inactivity: A sedentary lifestyle can exacerbate the risk factors for NAFLD, such as obesity and insulin resistance. Regular physical activity helps in managing weight, reducing liver fat, and improving insulin sensitivity.
Insulin Resistance and Type 2 Diabetes: These conditions are closely linked with NAFLD. Insulin resistance, where the body's cells don't respond effectively to insulin, can lead to an increased accumulation of fat in the liver.
Metabolic Syndrome: This is a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels, which together increase the risk of heart disease, stroke, and NAFLD.
Excessive Caloric Intake: Consuming more calories than the body can use can lead to excess fat storage in the liver. Monitoring and managing caloric intake can help prevent and manage NAFLD.
Rapid Weight Loss or Extreme Diets: While weight management is crucial for preventing NAFLD, rapid weight loss or following extreme diets can stress the liver, potentially exacerbating liver issues.
HOW IS NAFLD DIAGNOSED?
NAFLD is often diagnosed after noting abnormal liver function on blood tests, followed by some type of imaging study, such as a liver ultrasound. However, since NAFLD often presents with no symptoms, especially in its early stages, it can go undiagnosed for years. When symptoms do occur, they may include fatigue, weakness, and discomfort in the upper right abdomen.
HOW IS NAFLD TREATED?
Management and treatment of NAFLD typically focus on addressing the underlying risk factors, such as obesity and insulin resistance. Lifestyle changes, including a low fat, high fiber plant-predominant diet, weight loss, and increased physical activity, are the most recommended approaches. In more advanced cases, medications or surgery may be necessary, especially for those with NASH or cirrhosis.3
SUMMARY
Given its growing prevalence and potential to progress to more serious liver disease, NAFLD is a significant public health concern, highlighting the importance of early detection and proactive management. Lifestyle modifications can help prevent NAFLD and is the first line of treatment recommended for managing NAFLD, underscoring their importance in maintaining liver health and overall well-being.
🥦 Do you know about our STREAMING PLUS membership?
Our membership is built like a streaming service - you get a full library of plant-based cooking classes to watch whenever you want. PLUS, you gain access to upcoming interactive virtual cooking classes and a monthly accountability group call.
As a member you get:
Complete library of all past virtual classes - stream them whenever you’d like!
Free access to upcoming virtual classes
Library of easy and quick recipes: 100 and growing
Access to private Facebook group
Monthly accountability check-in and support group Zoom call with Caryn
Quarterly “Ask the Doc” call with Dr. Jim Loomis, our Medical Director
A community of support
To learn more, please visit us here.